Share this @internewscast.com
There’s nothing quite like summer in New York City. The birds fill Central Park, children laugh as they play in the spray from open fire hydrants, and the $20 sandwich from your favorite deli seems just right for a picnic along the waterfront.
It’s hard to ignore the fact that it’s as hot as the inside of a dog’s mouth. Without the option for weekend getaways to the Hamptons, navigating a subtropical New York City in the summer feels like a sequel to Les Miserables.
On my way to work, as sweat gathers on my upper lip and glistens above my eyebrows, I remind myself it could be worse. I could be experiencing a panic attack, something that was all too common for me before I found effective medication.
But then it hits – the very thing helping me keep my sanity in a crowded subway car is also the thing making me feel like I’ve been trapped in sauna fully clothed.
For about a decade, I’ve taken an SSRI – a selective serotonin reuptake inhibitor – to help with my anxiety and depressive episodes. Medications in this class include Zoloft and Prozac and among the laundry list of side effects, which include gastrointestinal issues, sexual dysfunction, and insomnia, is hyperhidrosis – or excessive sweating.
Of the roughly 32 million Americans take an antidepressant, around 21 percent – 6.7 million people – experience this less-than-ideal side effect, according to the International Hyperhidrosis Society. The excessive dampness occurs because SSRIs disrupt the body’s internal temperature gauge, triggering excessive – and sometimes unnecessary – sweating.
Dr Angela Downey, a family physician and host of the Codependent Doctor Podcast, told me that these medications impact the hypothalamus, also known as the brain’s thermostat, ‘which affects how your body regulates your body temperature and sweat production.’
She said: ‘Think of serotonin like an orchestra conductor who has suddenly turned up the volume on your internal HVAC system. It will sometimes overcorrect and can lead to unexpected sweating, especially at night or in warm weather.’

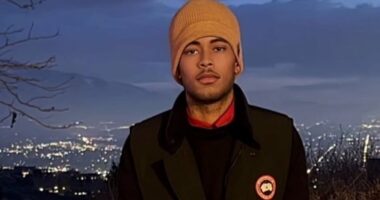
Me in the sweltering New York City summer featuring my trusty battery-powered fan that I take on the subway (and everywhere else)
What a trade-off. I don’t have crippling panic attacks or a dark cloud of gloom hanging over me, but after 10 minutes of walking down 8th Avenue, I look like I just crawled out of the East River.
Excessive sweating or hyperhidrosis is a relatively common side effect of SSRIs and another class of drugs similar to SSRIs that I’ve also taken called serotonin-norepinephrine reuptake inhibitors (SNRIs), which include Effexor and Cymbalta, according to Dr Olalekan Otulana, a general practitioner and addiction medicine specialist in the UK.
SSRIs allow serotonin – the ‘happy hormone’ to remain available in the brain’s synapses for longer before being reabsorbed, leaving more of the feel-good neurochemical around to improve mood and alleviate anxiety.
SNRIs block the reuptake of both serotonin and norepinephrine – a hormone that regulates the intensity of some emotions – increasing levels of both neurotransmitters to improve mood.
He told me that these drugs stimulate the body’s temperature regulation center.
This ‘can lead to the body perceiving that it is warmer than it is, triggering the sweat glands to produce more perspiration as a cooling response.’
The hypothalamus is the body’s thermostat, and the serotonin molecules there contain receptors that, when stimulated by an SNRI or an SSRI, can lower body temperature by promoting heat loss, including sweating profusely.

The graph shows antidepressant use in women, men, and both sexes together over the past 30 days in the US from 2009 to 2018
SSRIs flood the brain with serotonin, disrupting the hypothalamus’s ability to interpret temperature cues. It takes the influx of serotonin as a signal to start sweating.
And when you add norepinephrine in SNRIs to the mix, the hypothalamus gets a double hit of dysregulation and a direct impact on sweat glands.
Dr Ashwini Nadkarni, a board-certified psychiatrist at Mass General Brigham and Assistant Professor of Psychiatry at Harvard Medical School, told me: ‘To deal with this, people can discuss options with their treating physician,’ including switching to an antidepressant less likely to cause sweating, such as Vortioxetine.
‘Non-pharmacological strategies include wearing loose attire with breathable fabrics, keeping cool with a fan, and staying hydrated during the day,’ she said.
I have tried several different SSRIs and SNRIs in my long career in mental illness, and was never warned about hyperhidrosis. Psychiatrists were quick to warn a high-school-age me about low libido, though.
Dr Otulana added: ‘People often notice this side effect more in the summer as their baseline sweating due to heat is already higher. And the drug effect amplifies this.
‘For some, it can be quite distressing, especially if it affects confidence at work or in social situations.’
Indeed, few things irk me more than spending a pretty penny on high-quality makeup products only for them to slowly shift and melt on my face, so that by the time I enter work, I resemble a Picasso drawing.

Of the roughly 32 million Americans take an antidepressant like Zoloft (pictured), around 21 percent – 6.7 million people – experience this less-than-ideal side effect (stock)
Dr Darji added: ‘I always tell patients this is a real side effect and not something they’re imagining. It can impact their quality of life or make them want to stop their medication, which is why we take it seriously.’
If you find the sweating to be unbearable, don’t stop taking your medicine without the guidance of your doctor, who will begin tapering your dose safely to avoid unpleasant withdrawal symptoms.
‘Make sure you speak to your doctor about it. We can adjust the dose, switch to a different medication, or add a small dose of another medication to help manage the sweating,’ Dr Uma Darji, a board-certified family medicine physician, told me.
For millions of people, a sweaty summer (and fall, winter, and spring) is a small price to pay for emotional stability, or at least some semblance of it.