Share this @internewscast.com
Two sisters from North Carolina, both in their 20s, faced a harrowing journey as they were diagnosed with breast cancer just months apart, leading to the urgent decision of undergoing double mastectomies.
Kate and Elizabeth Singletary, who are triplets, discovered they both carry the CHEK2 gene mutation, known to significantly increase the risk of breast cancer, shortly before each received their diagnosis.
Kate Singletary, 27, a paramedic and medical student based in Winston-Salem, first noticed a lump in March 2024.
“I realized something was off with my breast,” she shared with WGRZ, describing the mass as “a pretty big lump.”
In an article for Women’s Health, she recounted the moment the doctors hinted at cancer: “When they first suggested it was cancer, I felt completely numb.
“I was nodding as the radiologist spoke, but I honestly tuned out most of what he said.”
A biopsy confirmed invasive ductal carcinoma, and doctors treated it as Stage III while assessing possible lymph-node and bone involvement.
‘Everything was happening so fast,’ she wrote, saying her team moved her directly into chemotherapy before surgery due to the suspected spread.

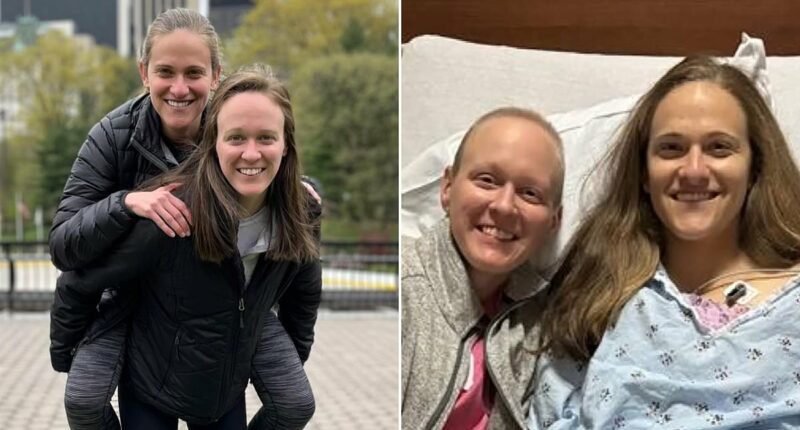
Kate and Elizabeth Singletary of Winston-Salem, both 27, were diagnosed with breast cancer within months of each other triggering an urgent double mastectomy

Kate first found a lump in her breast in March 2024 with Elizabeth being diagnosed 18 months later

The sisters are part of a set of triplets. They are both pictured here with their brother Jack
‘It’s crazy that you can take care of yourself and be healthy and this can still happen,’ Kate wrote.
In 2019, she had run 4,000 miles across the country to raise money for young adults with cancer.
Genetic testing then revealed she carried the CHEK2 mutation. Her sister Elizabeth was tested next – and her result also matched.
‘Mine came back positive for that genetic mutation as well,’ Elizabeth told WGRZ.
She underwent further scans and was diagnosed with Stage I breast cancer roughly half a year after Kate’s initial diagnosis.
Recalling the moment Elizabeth was told, Kate wrote: ‘I started crying. I didn’t want her to have to go through all of this too.
‘But she’s faced it with a lot of courage and grace, and told me that she would be much more scared about her diagnosis if she hadn’t seen me already go through chemo with a later-stage cancer.’
Both sisters proceeded with aggressive treatment plans. Each underwent a double mastectomy just five days apart as doctors worked to eliminate any remaining cancer and reduce future risk.
Kate said the proximity of their surgeries resulted in the sisters recovering ‘under the same roof,’ even helping one another manage surgical drains and post-operative care.
The Singletarys’ case has prompted doctors to warn young women about rising risks and the importance of early genetic screening.
Doctors say their experience illustrates how aggressive breast cancer can be in younger patients and how quickly families with inherited mutations can be impacted.
Atrium Health Wake Forest Baptist breast surgeon Dr. Marissa Howard-McNatt said the sisters’ case underscores the immediate need for early screening protocols among women with family history or known gene mutations.

Kate, a paramedic and medical-school student, first detected a lump in March 2024

Both women underwent a double mastectomy just five days apart as doctors worked to eliminate any remaining cancer and reduce future risk

Kate and Elizabeth Singletary of Winston-Salem, who are part of a set of triplets that includes brother Jack. They women learned they both carried the CHEK2 gene mutation – a mutation linked to elevated breast-cancer risk shortly before each received their own diagnosis

Both sisters are now cancer-free although Kate continues follow-up procedures to ensure there is no residual disease
‘Those individuals should undergo high-risk screening, meaning they should start mammograms at an earlier age, typically at least 10 years prior to the diagnosis of their first-degree relative,’ she told the North Carolina station.
High-risk monitoring includes alternating mammograms with MRIs.
Kate’s treatment moved at breakneck speed. She described 20 weeks of chemotherapy that drained her physically and shredded her emotionally.
‘I lost weight from anxiety, and I was constantly fatigued,’ she wrote. ‘I started losing my hair 12 days after starting chemo, and that’s when it felt real because I actually looked like a cancer patient.’
She and her mother cried together the day her head was shaved.
She tried to distract herself by working at a desk between shifts as a paramedic but isolation, fear, and intrusive thoughts never left her mind.
‘What if chemo doesn’t work? What if the cancer spreads? What if treatment works, but then the cancer comes back?’ she wrote.
Yet as the weeks passed, she could literally feel the tumor shrinking. ‘It was like it was melting away,’ she wrote.
She finished chemo on September 11.
In her account, Kate wrote that her cancer responded to chemotherapy, shrinking significantly before surgery but tests later showed cancer remaining in her lymph-node region, requiring another operation and six additional weeks of radiation.
Two weeks later, Elizabeth called with her own diagnosis.
‘While I don’t want her to go through this, it’s been nice to support each other through it and spend time together while we’re both living at home again,’ Kate wrote.
Both sisters are now cancer-free although Kate continues follow-up procedures to ensure there is no residual disease.
Their father previously battled multiple myeloma meaning the family has now faced three cancer diagnoses in six years.

Kate Singletary is seen alongside her mother and cancer doctors at the hospital

Kate is seen receiving treatment for breast cancer shortly after her diagnosis in early 2024

Kate is seen getting ready to ring the bell following her final round of treatment. She is pictured alongside her sister and parents
Kate wrote that the experience has pushed her to warn younger women to take screening seriously.
‘I want women to know that cancer doesn’t discriminate based on age,’ she wrote, urging monthly self-breast exams and early genetic testing especially if there’s family history.
‘If something feels different, you can get it checked out,’ she urges.
Doctors say they are increasingly finding more aggressive cancers in younger patients with families often learning their inherited risk only after the disease has already arrived.