Share this @internewscast.com
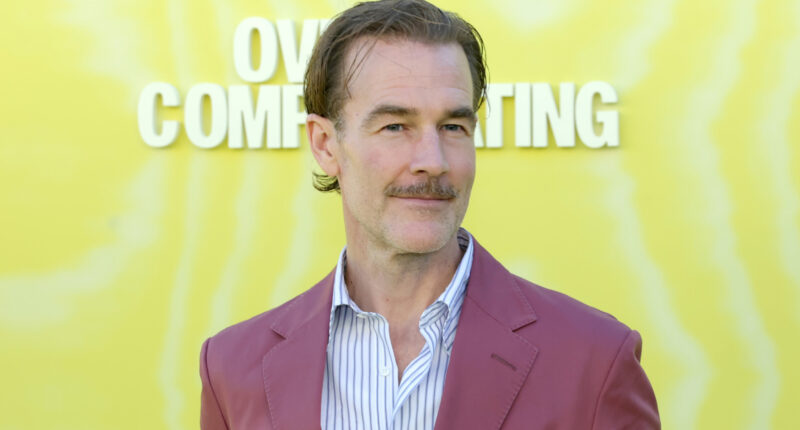
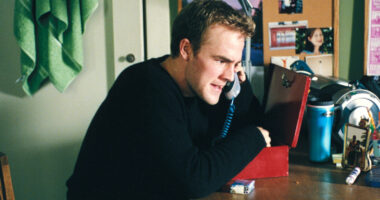
James Van Der Beek, fondly remembered for his iconic roles, passed away at 48 on February 11, 2026, following a battle with complications from colorectal cancer. While many recall him as Dawson Leery from “Dawson’s Creek” or Mox in “Varsity Blues,” Van Der Beek also made a brief appearance in the lesser-known 2017 film “Downsizing,” starring Matt Damon. In the movie, he played an anonymous anesthesiologist, an old high school acquaintance of Damon’s character, Paul Safranek, appearing during a reunion scene.
This casting choice might have been a nod to Van Der Beek’s fame from “Dawson’s Creek,” as “Downsizing” features cameos from other renowned actors like Neil Patrick Harris, Laura Dern, and Niecy Nash. The film follows Paul Safranek, an occupational therapist, who volunteers for an experimental procedure to shrink humans as a solution to climate change and overpopulation. Although his wife backs out at the last moment, leaving him to downsize alone, Paul discovers new opportunities in his miniature world.
Despite Van Der Beek’s involvement, “Downsizing” struggled to make an impact at the box office. Released in mid-December 2017, it faced stiff competition from blockbusters like “Star Wars: The Last Jedi,” “Jumanji: Welcome to the Jungle,” and “The Greatest Showman.” With earnings just over $55 million against a $68 million budget, it was deemed a financial disappointment. Critics and audiences alike were underwhelmed, labeling it one of Matt Damon’s less successful films, a sentiment that persists today.
The concept of miniaturization has been explored in cinema before. “The Incredible Shrinking Man” tackled this theme with a fantastical approach in 1957, while Lily Tomlin gave it a comedic twist in 1981’s “The Incredible Shrinking Woman.” Rick Moranis also achieved significant success with the 1989 family hit “Honey, I Shrunk the Kids.” These earlier films may have contributed to the lukewarm reception of “Downsizing.”
Downsizing flopped at the box office
While “The Incredible Shrinking Man” remains a sci-fi classic potentially ripe for a remake, and Moranis’s film continues to charm families, “Downsizing” has largely faded from public memory. However, James Van Der Beek’s enduring charisma and presence on both the big and small screens remain unforgettable, preserving his legacy in a way that is truly unshrinkable.
Perhaps audiences were less than enthusiastic about yet another film in which the protagonist is reduced to a fraction of their typical stature. “The Incredible Shrinking Man” mined this territory with a much more fantastic bent in 1957, Lily Tomlin put a comedic spin on it in 1981 for “The Incredible Shrinking Woman,” and Rick Moranis used a similar premise to score a massive hit with 1989’s “Honey, I Shrunk the Kids.”
While “The Incredible Shrinking Man” is a sci-fi classic that’s possibly due for a remake, and the Moranis movie is a family favorite, people have largely forgotten “Downsizing.” But they’ll never forget Van Der Beek’s warm, charismatic presence on the big and small screens. It is, in fact, unshrinkable.