Share this @internewscast.com
In the silent corridors of our bodies, cancer often hides its earliest signals, leaving them concealed in the bloodstream, experts say. Despite the absence of apparent symptoms, these early indicators can provide crucial warnings long before a formal diagnosis is made.
During your next medical visit, it’s likely that healthcare professionals will suggest routine blood tests. These assessments aim to detect potential issues such as increased cholesterol levels, irregularities in blood sugar, and liver enzyme changes, among other vital health metrics.
Many times, by the moment visible symptoms of cancer emerge, the disease has been silently progressing for years. Clues to its presence may have already appeared in blood tests. For example, an increase in fasting insulin might indicate metabolic issues, while high levels of C-reactive protein (CRP) could suggest chronic inflammation, often linked with nutrient shortages.
Dr. Elias Obeid, serving as the Medical Director at the Hennessy Institute for Cancer Prevention & Applied Molecular Medicine in New Jersey, explained to the Daily Mail, “As an oncologist focusing on cancer genetics and prevention, I can attest that subtle changes in routine blood markers, like ferritin and fasting glucose, may precede a cancer diagnosis. However, interpreting these changes is complex and highly contextual.”
These subtle indicators are frequently overlooked. Individually, they might appear trivial, yet collectively they outline a concerning picture: metabolic disruption, persistent inflammation, impaired cellular communication, and an overburdened immune system. Such an environment is conducive to cancer’s development and growth.
Elevated CRP levels, for instance, suggest that inflammatory molecules such as cytokines are beginning to inflict DNA damage, encouraging cell proliferation and division. This process, in turn, fosters the growth of blood vessels that tumors exploit for nourishment.
Ferritin is a protein that stores iron and releases it when needed. Abnormal levels signal a disruption in this balance. Too much iron triggers oxidative stress, producing free radicals that damage DNA and cell membranes – a known cancer trigger. Too little iron starves the immune system, weakening the natural killer cells that patrol for threats. Both extremes leave the body dangerously exposed.
Some cancers, such as low-grade breast cancer, can develop and remain asymptomatic for five to 10 years before symptoms manifest. But recent research has found that blood testing can detect genetic material shed by tumors in the bloodstream several years before a cancer diagnosis, giving people time for early intervention.

When you visit a doctor, blood work is routine, offering insights into everything from blood cell counts and organ function to cholesterol levels. But these standard tests can also reveal early cancer clues years before symptoms appear (stock)
Dr Obeid said: ‘It is a common scenario in my practice to see patients who, in retrospect, had subtle but concerning trends in their routine bloodwork for years before their cancer diagnosis. A classic example is a patient diagnosed with pancreatic cancer.
‘Looking back at their records from the preceding two to three years, we might see a new and unexplained rise in their fasting glucose, sometimes even leading to a new diagnosis of diabetes in someone with no other risk factors.
‘At the time, this may have been treated as a metabolic issue, but it was actually the first sign of the developing tumor.’
Pancreatic cancer is usually diagnosed late, often after it has spread to other organs.
Because the pancreas is tucked behind other organs and early symptoms are often vague or absent, roughly 82 percent of cases are diagnosed only after the cancer has spread. This late detection typically renders tumors inoperable, leading to a grim prognosis.
The cancer is also becoming more prevalent in people under 55.
Between 2000 and 2021, pancreatic cancer diagnoses increased by 4.3 percent per year among Americans aged 15 to 34, and by 1.5 percent annually among those aged 35 to 54, according to a 2025 analysis.
Though the absolute numbers remain small, specialists say the trend is nonetheless concerning.
![Dr Obeid [not pictured] cautioned that these markers aren't definitive cancer screens for the general population, but rather pieces of a larger puzzle. A patient might show a slow, progressive drop in hemoglobin and red blood cell size over years, a developing anemia (stock)](https://i.dailymail.co.uk/1s/2026/02/21/17/106550227-15558799-Dr_Obeid_not_pictured_cautioned_that_these_markers_aren_t_defini-a-20_1771695295747.jpg)
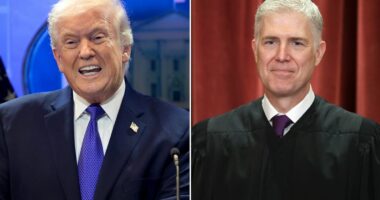
Dr Obeid [not pictured] cautioned that these markers aren’t definitive cancer screens for the general population, but rather pieces of a larger puzzle. A patient might show a slow, progressive drop in hemoglobin and red blood cell size over years, a developing anemia (stock)
During an annual checkup, doctors may take a blood sample to measure the complete blood count (CBC).
An abnormal white blood cell count may signal infection. Low red blood cells indicate anemia. And low platelets can point to underlying issues with the bone marrow, including leukemia or lymphoma.
A comprehensive metabolic panel (CMP), meanwhile, measures 14 different substances from enzymes to proteins in a blood sample to review liver and kidney function, metabolism and the balance of electrolytes to fluids.
Doctors’ reference ranges are statistical constructs based on large populations. They indicate with is ‘average,’ not what is optimal for you and your long-term health.
A fasting insulin of eight µIU/mL might technically be ‘normal,’ which is typically under 25, but if your personal baseline has been rising for a few years, the creep up to eight is a meaningful signal of insulin resistance, a condition in which muscle, fat and liver cells do not respond to insulin, forcing the pancreas to overproduce it to keep blood sugar in check.
Even slight deviations over time in these metrics within or slightly outside of the normal range can indicate a brewing problem.
Dr Obeid said: ‘These are not definitive cancer screening tools for the general population, but rather pieces of a larger puzzle.’
He also added that a ‘patient might have a slow, progressive drop in their hemoglobin and red blood cell size over several years – a developing microcytic anemia,’ a condition where red blood cells become smaller than normal and carry less hemoglobin, often resulting from iron deficiency.
![Dr Obeid [pictured] noted that for healthy individuals, standard annual tests like a CBC, metabolic panel and lipid panel offer a useful snapshot of organ function and metabolic health, but stressed they are not designed for proactive cancer screening](https://i.dailymail.co.uk/1s/2026/02/21/17/106528797-15558799-Dr_Obeid_pictured_noted_that_for_healthy_individuals_standard_an-a-21_1771695295773.jpg)
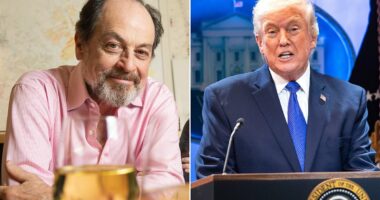
Dr Obeid [pictured] noted that for healthy individuals, standard annual tests like a CBC, metabolic panel and lipid panel offer a useful snapshot of organ function and metabolic health, but stressed they are not designed for proactive cancer screening
While most commonly caused by blood loss or poor diet, anemia can sometimes signal something more serious.
In older adults, unexplained or slowly worsening microcytic anemia may indicate internal bleeding from a gastrointestinal tumor, such as colon cancer, or chronic inflammation driven by malignancy.
‘Because the drop is gradual and the values may stay within the low end of the “normal” range for a long time, it’s often not investigated until the anemia becomes severe and the patient develops symptoms.’
A gradual drop in hemoglobin from the average of 13.5 to 11.8 g/dL, meanwhile, could indicate a drop in blood marrow activity – reducing the production of blood cells – or nutrient insufficiency long before a doctor can diagnose anemia.
More specific blood tests, such as the multi-cancer early detection (MCED) test, check blood and saliva samples for signs of multiple types of cancer, including pieces of DNA and RNA shed by tumors.
One type of MCED test can detect cancer signals from more than 50 different cancer types. This includes the 12 cancers responsible for roughly two-thirds of all cancer deaths in the US, such as lung, colorectal, pancreatic and liver.
The MCED isn’t part of a normal blood panel, though. It’s something a patient has to ask for a doctor to prescribe. Even then, spotty insurance coverage and high costs pose a significant barrier to obtaining the test.

The above chart shows the survival rate of pancreatic cancer by stage
Without insurance, a standard blood test, which includes basic testing, a CMP and a lipid panel, costs around $25. But comprehensive panels can add up to the hundreds without insurance. For example, an iron profile, which measures total iron levels, can cost up to $200.
A Vitamin D test runs up to $250 while specialized thyroid tests range from $225 to $275. With insurance, costs can dip far lower to roughly $30.
Still, doctors argue that these are small prices to pay for powerful insights into your body and its defenses against chronic diseases, alongside regular screenings.
Dr Obeid said: ‘For any healthy individual, the standard annual panel – including tests like a Complete Blood Count (CBC), Comprehensive Metabolic Panel (CMP), and a lipid panel – provides a valuable snapshot of your current organ function and metabolic health. However, it is not designed for proactive cancer screening.
‘The first step in proactive screening is to better understand your personalized cancer risk.’