Share this @internewscast.com
A PHOTOGRAPH in the family home of late football legend Gordon McQueen shows him leaping high into the air to head the ball.
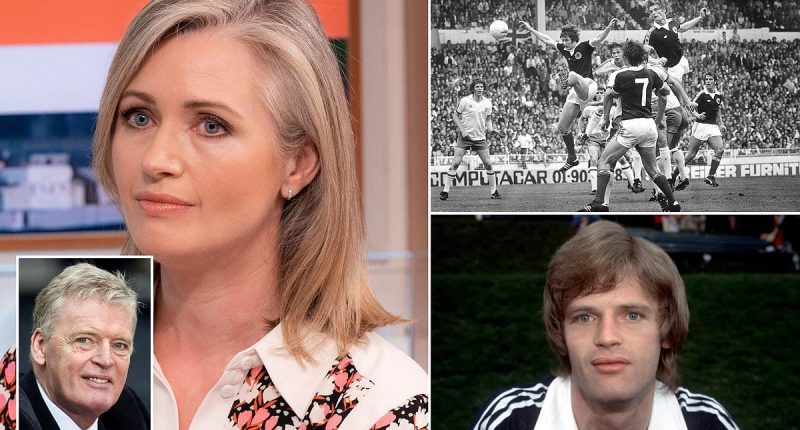
It’s an image which elicits a range of emotions in his daughter Hayley McQueen.
She remains proud of her father’s illustrious career and the many special moments like that in the photograph when the ex-St Mirren, Leeds United, Manchester United and Scotland defender was at the peak of his physical prowess.
Sky Sports presenter Ms McQueen said: ‘I suppose maybe I do look at (the artwork) slightly differently now, but I don’t look at it with anger and it doesn’t make me too upset.
‘It’s just quite saddening to look at it, to think, “Well, that is what took dad’s life so early”, but that is also what gave us so much.’

Gordon McQueen scores a header for Scotland against England at Wembley in 1977

Hayley McQueen admits to feeling ‘bittersweet’ about her late father’s career in football
Following a post-mortem on her father, a coroner ordered an inquest to probe whether there was a link between his illness and his playing career.
The family have spoken of their fear that there is a connection, with Ms McQueen, 45, stating she expects worse to come.
She said: ‘I think we’re facing an epidemic. In a few years, there are going to be not just hundreds, but possibly thousands, of footballers affected. And I don’t just mean professionals who played at the top of the tree. Right across the football leagues there will be a lot of footballers suffering with neurodegenerative disease.’
Asked if other ex-players speak to her about the issue, she said: ‘Yes, loads. I know a very, very high profile, former Manchester United player who used to get headaches and migraines and has elements of forgetfulness now.
‘He’s obviously worried. I said, “Well, why don’t you just go and get a test? Why don’t you go and get a scan?” But he said, “I don’t want to. I don’t think I want to know”. That’s awful.’
Such is their commitment to exploring the issue, McQueen’s family donated his brain to research being conducted by Professor Willie Stewart, a consultant neuropathologist at Glasgow University and a leading expert in brain injury in sport. His analysis found Chronic Traumatic Encephalopathy (CTE) — a brain condition thought to be linked to repeated head injuries and blows to the head.

Gordon McQueen died in June 2023 after a battle with vascular dementia

McQueen worked as a TV pundit following his playing career with St MIrren, Leeds and Manchester United
The NHS states that CTE slowly gets worse over time and leads to dementia. This played a part in the coroner’s decision to hold the inquest into McQueen’s death. At present, the hearing has been postponed because medical records compiled by doctors at the clubs McQueen played for between 1972 and 1985 are missing.
However, there is nothing in the records they do have to suggest injuries outside of football, such as a car crash or assault, that might have resulted in brain damage.
Ms McQueen said: ‘With all the medical evidence and research out there right now, everything points to heading a football.
Particularly, the position that my dad played, at centre-half, seems to have a higher amount of players that have dementia. They were defenders, and my dad was a prolific header of a football.’
The Sky Sports presenter said the family don’t plan to take legal action against football authorities if a link between her dad’s illness and the sport is determined.
However, she hopes to raise awareness of the risks associated with heading the ball. She is also grateful for the role played by the Scottish FA in bringing their English counterparts into the inquest process.
She said: ‘The SFA were present in the two pre-inquest hearings, as well as representatives from Leeds United and Manchester United. The FA, who we thought would be a party of interest, didn’t express an interest.
‘However, the SFA got in touch with the FA to say that they felt because my dad’s playing career essentially was in England that the FA should be part of any hearing. Therefore the FA were there at the last meeting that we had and that was actually the SFA who made that happen.’
Ms McQueen said the delay to the inquest and the questions that remain over what caused her father’s illness have made the grieving process harder. The family buried half of his ashes in the graveyard of the Yorkshire village of Hutton Rudby, where he lived until his death.
They planned to wait until the inquest concluded to scatter his remaining ashes at his first club — Kilbirnie Ladeside — in the Ayrshire town where he was born and grew up.
However, they now plan to do this as soon as they can organise for their whole family to be together.
Ms McQueen said: ‘The football club is literally round the back of the house where my grandad lived on Glenriddet Avenue, and they had a big, long garden that looks on to the pitches.
‘Kilbirnie Ladeside said they would allow us to go down and scatter his ashes in a little bit of land near where some of the pitches are.’
The second anniversary of McQueen’s death on June 15, 2023, falls on Father’s Day this year, adding another element of sadness to what will already be a difficult day for his daughter and the rest of the family.

McQueen hopes to raise awareness of the risks associated with heading the ball
It may be two years later, but the memory of her father’s heartbreaking decline remains.
Ms McQueen said it was a feeling that her father was being ‘hidden away’ as they cared for him and kept his illness private that eventually led them to discussing his condition openly.
She said: ‘We only came out and spoke about his dementia because we still had people asking him to do radio interviews and attend after-dinner speeches, and we still had people sending stuff for my dad to sign and he couldn’t. He couldn’t write. He couldn’t sign his name anymore.

Gordon McQueen won 30 international caps for Scotland, scoring five goals
‘The only reason we came out was because I felt like my dad had been hidden away for a year or two. I guess we needed to let people know why it seemed like he had disappeared. And then I realised I was really happy that we did that.’
Ms McQueen said her family had been told in December 2022 that her father had ‘weeks, if not days’ left to live.
However, his body proved so strong despite the progression of the disease that he lived for another six months.
She said: ‘With a lot of sports people, their brain is fighting against their body. These guys kept their bodies fit and healthy.’
The wait for the inquest goes on, but for now, Ms McQueen and her family take strength from the fact they are not alone.
She said: ‘There’s a little bit more noise now, and people actually speaking out about their worries in football right now. There are a lot more footballers with dementia than you can even imagine.’