Share this @internewscast.com
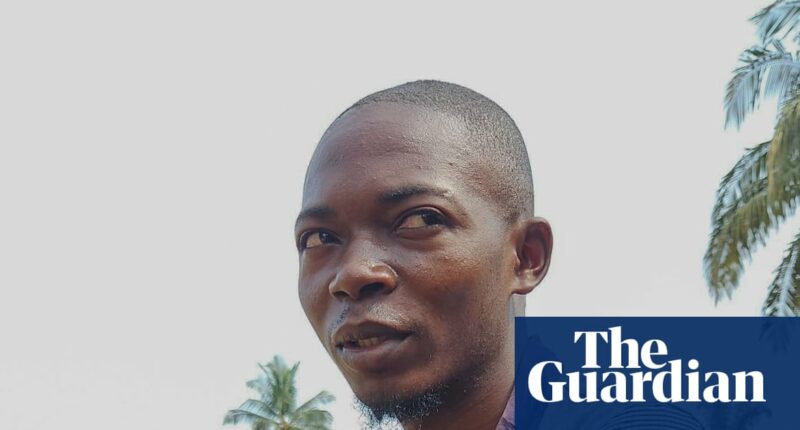
Bope Mpona Héritier experienced a series of unimaginable losses when his two-year-old daughter passed away, followed by his mother and then his wife. Yet, he remained in the dark about the illness that claimed their lives. It wasn’t until Héritier, at 25, began to exhibit symptoms himself that the mystery was solved. His blood test, sent to Kinshasa, the Democratic Republic of the Congo’s capital, confirmed he had contracted the Ebola virus.
“The pain was everywhere,” he recounts. “I suffered from a migraine and sharp pains in my eyes and throat, along with severe vomiting. My appetite vanished, and I lost significant weight as a result.”
The remote community of Bulape in Kasai province never anticipated the arrival of a deadly virus like Ebola. Yet, on September 4th of this year, the health ministry declared an outbreak—the nation’s 16th. By September 14th, there were 35 confirmed cases, including 16 fatalities, some among healthcare workers. A concerted effort by various agencies was launched to contain the outbreak.
With the last patient discharged on October 19th, healthcare workers and residents of Bulape are cautiously optimistic about an impending all-clear. If no new cases emerge within 42 days, the outbreak could officially be declared over by early December.
However, reaching this milestone has been anything but easy.
Ebola, while rare, is a severe viral disease that initially causes fever, fatigue, and muscle aches. As it progresses, “wet” symptoms like vomiting, diarrhea, and often internal and external bleeding manifest.
It is transmitted to people from wild animals, such as fruit bats and primates, and spreads through the body fluids of those infected. It is often fatal if untreated.
Since the virus was discovered in 1976, there have been 16 outbreaks in the DRC, according to the US Centers for Disease Control and Prevention (CDC). The most recent large-scale outbreak, the largest in the DRC’s history, occurred in North Kivu and Ituri between 2018 and 2020. It was the world’s second-largest outbreak after one in west Africa between 2014 and 2016 which spread across a number of countries, infecting more than 28,600 people and killing 11,325.
The latest outbreak was complicated by the remoteness of the affected area. “It took some of us four days to reach Bulape from Kinshasa because we had to cross forests,” recalls Chiara Montaldo, the medical response coordinator in Kasai for Médecins Sans Frontières (MSF). “We had to bring everything from outside, like medicines, materials for building tents, even water-decontamination supplies,” she says.
Shortly after reaching the affected area, medics from MSF, the World Health Organization and the DRC’s health ministry established a 32-bed Ebola treatment centre at Bulape general hospital, where Héritier was admitted.
“I had passed out by the time we got there, so I didn’t know where I was,” he says. “I received treatment early and was vaccinated, so MSF told me I had a better chance at surviving than many others.”
Bulape’s isolation, while a logistical nightmare, has also helped keep the virus local. By contrast, the 2014–16 outbreak in west Africa quickly spread across three countries.
Montaldo says: “The numbers for that outbreak were on a magnitude we couldn’t imagine for Ebola. In North Kivu, the numbers were big too, but there the main challenge was the conflict [between armed groups in Ituri and North Kivu].”
after newsletter promotion
Reaching a remote region such as Bulape was not the only challenge. Unlike in North Kivu, there was also a severe shortage of human resources.
“A problem we faced early on was that there were not enough local nurses or doctors trained to deal with an Ebola outbreak,” Montaldo says. “Of course, we come with an international team, but we try to recruit locally. Eventually, we managed to build a team mainly made up of local staff.”
As infection rates continued to rise through early and mid-September, the fight against Ebola became an emotional one – for health workers and patients – as well as a medical battle.
“In the tent I was in, there were three other patients. I watched them all die, one by one,” Héritier says.
Even for veterans of outbreaks, such as Montaldo, the virus’s high mortality rate can make the medics’ efforts seem hopeless at times. “Here, we know that even if we treat people the best way we can, they might still die,” she says.
For survivors, the trauma lingers. “What else did I have to live for?” Héritier asks. “I wanted to kill myself, but I didn’t even have the strength to do that.”
MSF provided patients with psychological support – a lifeline for Héritier. “I spoke with a psychologist a lot, and he encouraged me to keep fighting. He gave me the belief that I could conquer Ebola. He told me: ‘Just because they died doesn’t mean you have to.’”
While treating patients who had contracted the disease, MSF and its partners on the ground also quickly mobilised to vaccinate more than 35,000 people in the region.
“It’s something we haven’t had in the past, and it definitely helped reduce the infection rate,” Montaldo says.
A total of 19 patients with the virus recovered out of 64 confirmed or suspected cases; there have been 45 deaths so far.
Héritier was among the lucky ones, but returning home has not been easy. “A lot has changed in my life,” he says. “Some of my friends are too scared to come near me because they think I’ll infect them. I think eventually they’ll forget, and things will go back to normal.”
Now, as he prepares to return to work on his farm, Héritier remains hopeful. “People shouldn’t be scared of diseases,” he says. “We have to trust that doctors will help us and not live in fear. I am proof of that.
“I was sick and unable to walk, and yet here I stand.”