Share this @internewscast.com
WASHINGTON — The U.S. has given the green light to the world’s only biannual injection for HIV prevention, as announced by Gilead Sciences on Wednesday. This marks the initial phase of a global launch intended to safeguard millions, though it’s uncertain how widely accessible this groundbreaking option will be both domestically and internationally.
NOTE: The video is from a previous report.
While a vaccine to ward off HIV is still necessary, some experts believe that this injection, known as lenacapvir, could be a significant alternative. It nearly eradicated new infections in two pivotal studies involving high-risk individuals, outperforming the daily preventive pills that can be easily forgotten.
“This really has the possibility of ending HIV transmission,” said Greg Millett, public policy director at amfAR, The Foundation for AIDS Research.
Although condoms are effective in preventing HIV when used correctly, PrEP—using preventive medications like daily pills or a bimonthly injection—is becoming increasingly significant. Lenacapavir offers six months of protection, making it the longest-lasting method available. It may appeal to those hesitant about more frequent medical appointments or concerned about the stigma associated with daily medication intake.
But upheaval in U.S. healthcare – including cuts to public health agencies and Medicaid – and slashing of American foreign aid to fight HIV are clouding the prospects.
Millett said “gaping holes in the system” in the U.S. and globally “are going to make it difficult for us to make sure we not only get lenacapavir into people’s bodies but make sure they come back” even as little as twice a year.
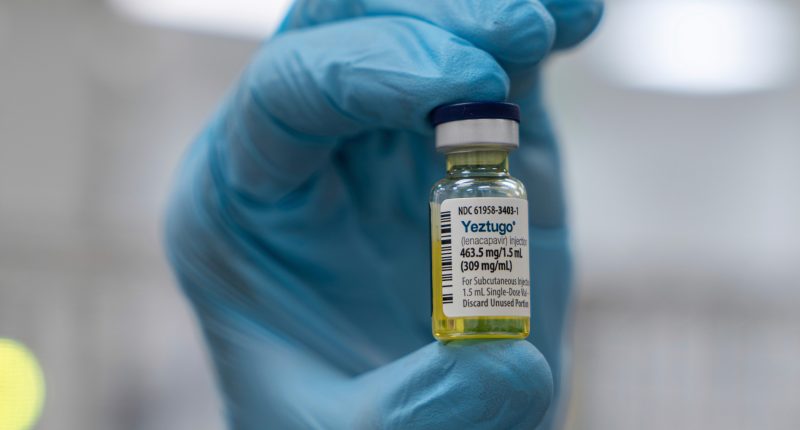
Gilead’s drug already is sold to treat HIV under the brand name Sunlenca. The prevention dose will be sold under a different name, Yeztugo. It’s given as two injections under the skin of the abdomen, leaving a small “depot” of medication to slowly absorb into the body.
Gilead didn’t immediately announce its price. The drug only prevents HIV transmission – it doesn’t block other sexually transmitted diseases.
Global efforts at ending the HIV pandemic by 2030 have stalled. There still are more than 30,000 new infections in the U.S. each year and about 1.3 million worldwide.
Only about 400,000 Americans already use some form of PrEP, a fraction of those estimated to benefit. A recent study found states with high use of PrEP saw a decrease in HIV infections, while rates continued rising elsewhere.
About half of new infections are in women, who often need protection they can use without a partner’s knowledge or consent. One rigorous study in South Africa and Uganda compared more than 5,300 sexually active young women and teen girls given twice-yearly lenacapavir or the daily pills. There were no HIV infections in those receiving the shot while about 2% in the comparison group caught HIV from infected sex partners.
A second study found the twice-yearly shot nearly as effective in gay men and gender-nonconforming people in the U.S. and in several other countries hard-hit by HIV.
Ian Haddock of Houston had tried PrEP off and on since 2015 but he jumped at the chance to participate in the lenacapavir study and continues with the twice-yearly shots as part of the research follow-up.
“Now I forget that I’m on PrEP because I don’t have to carry around a pill bottle,” said Haddock, who leads the Normal Anomaly Initiative, a nonprofit serving Black LGBTQ+ communities.
“Men, women, gay, straight – it really just kinds of expands the opportunity for prevention,” he added. Just remembering a clinic visit every six months “is a powerful tool versus constantly having to talk about, like, condoms, constantly making sure you’re taking your pill every day.”
“Everyone in every country who’s at risk of HIV needs access to PrEP,” added Dr. Gordon Crofoot of Houston, who helped lead the study in men. “We need to get easier access to PrEP that’s highly effective like this is.”
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education and the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
Copyright © 2025 by The Associated Press. All Rights Reserved.