Share this @internewscast.com

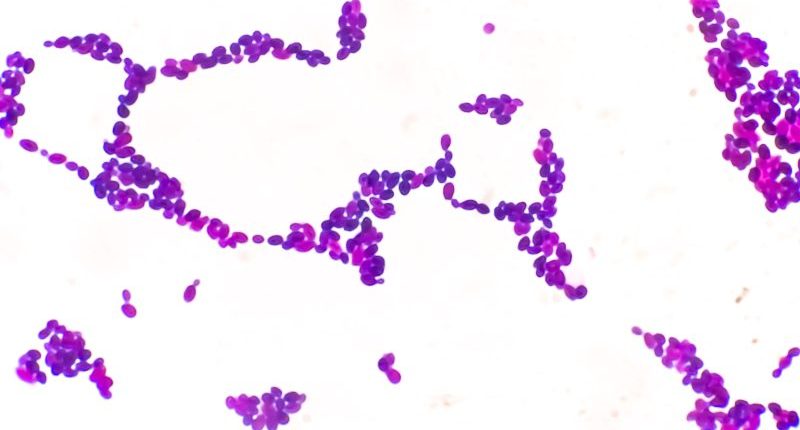
(NEXSTAR) – The deadly and drug-resistant fungus Candida auris is under close surveillance as health experts work to calm its spread.
In the United States, Candida auris, also known as C. auris, was initially identified less than a decade ago. Since its discovery, the number of cases has consistently risen each year.
In 2025, the emergence of new Candida auris cases appears to be comparable to this time last year, based on data submitted to the Centers for Disease Control and Prevention. Nonetheless, certain states are experiencing significantly higher numbers of cases compared to others.
Out of the 1,052 cases reported to the CDC thus far in 2025, around 25% have occurred in Texas. The Lone Star State has documented 241 cases of Candida auris as of late April, according to the most recent data from the CDC.
Other states seeing the fungus in large numbers include Michigan (185), Ohio (125), Virginia (99) and Arizona (98). Colorado, Delaware, Illinois, Indiana, Iowa, Louisiana, Maryland, Montana, New Mexico, Pennsylvania, Utah and Wisconsin have also all reported new cases this year.
The case counts are provisional, the CDC notes, and subject to change as more information becomes available.
The CDC has considered the fungus “an urgent antimicrobial resistance threat” because it has developed ways to defeat the drugs that are designed to kill it. When antifungal medications aren’t effective, the fungus can spread more easily and infections can be hard or even impossible to treat.
People with a healthy immune system may be able to fight off infection on their own, but Candida auris mainly spreads in health care settings, where people are sick and vulnerable.
People with catheters, breathing tubes, feeding tubes and PICC lines are at the highest risk because the pathogen can enter the body through these types of devices.
The fungus can survive on surfaces, like countertops, doorknobs, or even people’s skin, for a long time before spreading to vulnerable patients.
“It’s really good at just being, generally speaking, in the environment,” Melissa Nolan, an assistant professor of epidemiology and biostatistics at the University of South Carolina, told Nexstar.“ So if you have it on a patient’s bed for example, on the railing, and you go to wipe everything down, if in whatever way maybe a couple of pathogens didn’t get cleared, then they’re becoming resistant. And so over time, they can kind of grow and populate in that hospital environment.”
In the past, the CDC estimated that “based on information from a limited number of patients, 30–60% of people with C. auris infections have died. However, many of these people had other serious illnesses that also increased their risk of death.”